Correlation Between Polycystic Ovary Syndrome (PCOS) and Depressive Symptoms
PAIN TO POWER - Research paper by Kailyn Park
Abstract
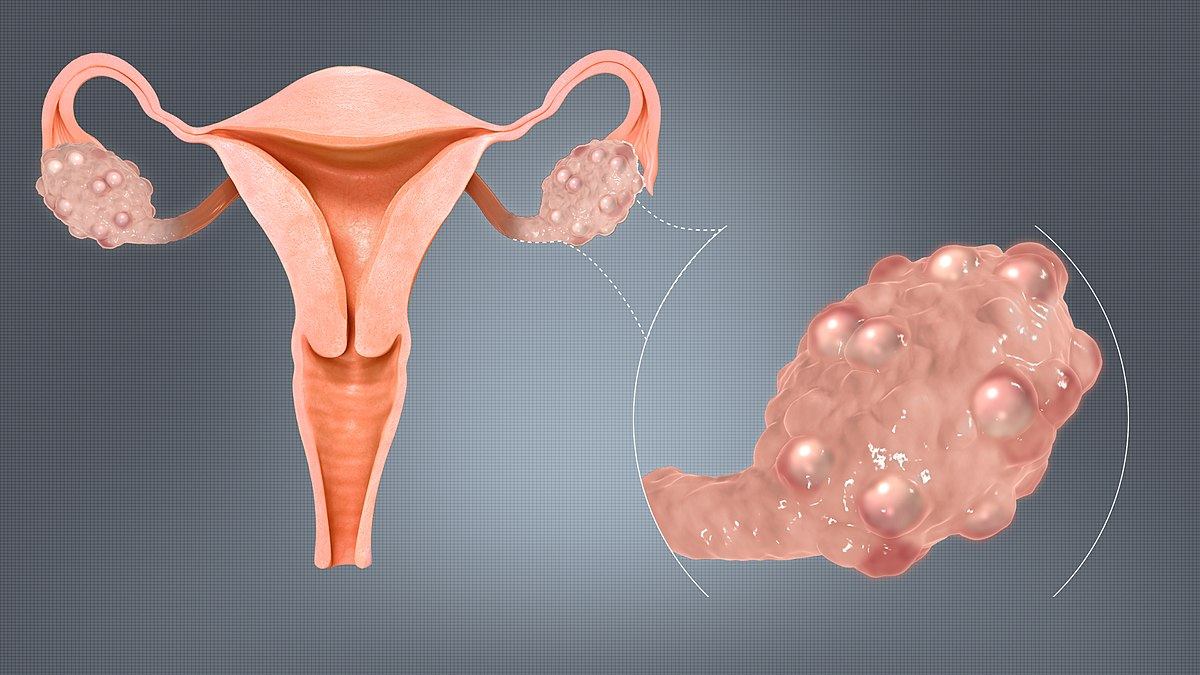
Polycystic ovary syndrome, also known as PCOS, is a hormonal condition in which cysts containing follicles develop in the ovary. Common symptoms of this condition include insulin resistance, stress, sleep apnea, infertility, and inflammation. Despite not being documented symptoms of PCOS, many women diagnosed with PCOS also report experiencing depressive symptoms. An electronic systematic literature review was conducted via PubMed and other medical organizations to determine the link between polycystic ovary syndrome and depressive symptoms. Results indicated that symptoms of PCOS can contribute to depression by disrupting one’s self-esteem and female identity. These findings raise important implications for methods of relieving these symptoms through therapeutic approaches to overcome the potential disruptions to one’s self-esteem and female identity.
Introduction
Polycystic ovary syndrome is a hormonal condition in which cysts, small sacs with fluid, contain follicles, or immature eggs. PCOS is a chronic disease, and there are numerous treatments on the market designed to alleviate a wide array of symptoms. To be diagnosed with PCOS, two of the three listed indicators must be present: excess androgen, irregular menstruation, or polycystic ovaries. The symptoms of PCOS include insulin resistance, stress, sleep apnea, infertility, and inflammation (Polycystic Ovary Syndrome (PCOS) - Symptoms and Causes, n.d.).
Depression is defined as a mental disorder in which an individual’s thoughts, feelings, behaviors, and sense of well-being are affected (World Health Organization: WHO & World Health Organization: WHO, 2023). Research indicates that women with PCOS tend to show higher rates of depressive symptoms (Dybciak et al., 2023). However, the direct cause and relationship between PCOS and depression are unknown. Some research suggests that the higher rates of depressive symptoms may be the byproduct of hormonal changes and/or symptoms such as infertility (Xing et al., 2022). Another potential explanation is the impact of additional underlying health conditions, such as type 2 diabetes (Castro, 2024).
There is no definitive connection between PCOS and depressive symptoms; however, there are some hypotheses that may explain their relationship. For example, some researchers hypothesize that the depletion of neurotransmitters such as GABA, acetylcholine, serotonin, etc., results in depressive moods (Xing et al., 2022). Additionally, telltale symptoms such as infertility, obesity, and irregular menstruation may potentially alter a person’s self-image and self-perception (Gnawali et al., 2021). The link between Polycystic Ovarian Syndrome and depressive symptoms is unclear; however, common symptoms include insulin resistance, stress, sleep apnea, infertility, and inflammation, which can heighten symptoms of depression through hormonal changes and neurotransmitters.
Literature Review
Type 2 Diabetes and Insulin Resistance
Type 2 diabetes is a documented potential long-term side effect of PCOS. Insulin resistance can raise blood sugar levels, and studies have shown that people who experience insulin resistance and type 2 diabetes are more prone to depression. Furthermore, the hypothalamic-pituitary-adrenal (HPA) axis is hyperactive in those with diabetes (Xing et al., 2022). The hyperactivity of this axis results in excess cortisol and disruption of glucoregulatory mechanisms (Xing et al., 2022). Glucoregulatory mechanisms ensure that blood glucose levels are within the normal range. The disruption of this mechanism can result in diabetes and obesity (Xing et al., 2022).
Common Symptoms: Infertility, Irregular Menstruation, and Obesity
The most common symptoms of PCOS consist of infertility, irregular menstruation, obesity, and infertility. 40-80% of women with PCOS are obese (Sam, 2007), 40-50% struggle with infertility (Melo et al., 2015), and 75%-85% experience irregular menstruation (Harris et al., 2017). Many of these women have also reported having a lower self-image and self-esteem. Lower self-esteem and self-confidence are strongly associated with depressive symptoms (Gnawali et al., 2021). Furthermore, infertile women may report higher levels of depressive symptoms and a lack of self-confidence because of their inability to experience “true” womanhood. Each person has their own set of values, but many are surrounded by the stereotypes and pressures of having children of their own. In addition to personal desires, pressures from society, family, and socioeconomic standards may also contribute to the lack of self-confidence (Xing et al., 2022).
Dysfunctioning Hormones and Neurotransmitters
Dysfunctional hormones and neurotransmitters can lead to the disruption of homeostasis and may lead to a negative feedback loop, which may ultimately contribute to depressive symptoms. In these cases, serotonin, GABA, and acetylcholine are diminished, which are associated with lower moods and depression. In these circumstances, cortisol, a steroid hormone that helps the body respond to stress, is excessive and leads to a desensitization of cortisol receptors (Xing et al., 2022). In addition to high cortisol levels, excess androgen is produced. Hyperandrogenism results in obesity, acne, and hair loss, which can alter a person’s self-image (Gnawali et al., 2021).
Method
Article Selection and Procedures
A systematic literature review was conducted to investigate the relationship between Polycystic Ovary Syndrome and depression. Electronic searches were used to retrieve articles and papers.
Search Procedures
This study conducted an extensive electronic search on Google Scholar, PubMed, and other medical organizations such as the Mayo Clinic and Columbia School of Nursing. The peer-reviewed articles were published from 2014 to 2023 using the following search items: Polycystic ovary syndrome, depression, depressive behaviors, and hormonal effects of PCOS. Other common mental disorders, such as anxiety, were not included. A total of seven articles were obtained electronically.
Inclusion and Exclusion Criteria
To be included, the article had to explain the symptoms of Polycystic Ovary Syndrome. Additionally, articles that detailed neurotransmitters, specific parts of the brain, and hormones were selected.
Discussion
This systematic review aimed to investigate the relationship between polycystic ovary syndrome and depression. An analysis was done with both the experimental group (patients with PCOS) and the control group (healthy patients). The data was gathered and analyzed from different countries and cultures. Additionally, the Hospital Anxiety and Depression Scale (HADS) was utilized to give the average HADS scores per sample, measuring depression and anxiety in those with physical illnesses (Lichtenberg, P.A., 2010).
In all six studies, there was a greater HADS-D score in the PCOS sample than in the healthy (control) group. This can be an indicator that there is a positive association between PCOS and depression. The most significant difference between the PCOS sample and the control group is the study done by Barry in 2011 in the United Kingdom. The difference in the HADS-D Score between the study group and the control group was 2.12. The most minor difference between the two groups was a study done by Dag in 2017 in Turkey, in which the HADS-D score difference was 0.24. The findings suggest that PCOS does have effects on mental health, specifically depression.
The most significant percentage of the sample with depression was in Tariq’s study in 2021. Out of the 137 PCOS patients who participated in the survey, 55.6% of patients reported symptoms of depression. On the other hand, the smallest percentage of the PCOS sample was Radhakrishan’s study, published in 2018, in which 16% of PCOS patients experienced depression. Moreover, according to the World Health Organization, 6% of the female population experiences depression.
Compared to the average population of women, more women who experienced PCOS also experienced depressive symptoms (Dybciak). One potential explanation for this is the impact of the symptoms often associated with PCOS. Infertility, irregular menstruation, and obesity, which are the most common symptoms used to diagnose this syndrome, can lead to a diminishing womanhood experience for many. This comes as a result of societal pressures in which a large stereotype associated with being a woman is having children and raising a family. As a result, the inability to have children can lower self-esteem and diminish the quality of life for these women (Xing et al., 2022).
Furthermore, diminished levels of neurotransmitters such as serotonin, GABA, and acetylcholine can also decrease mood and contribute to depressive moods. An excess release of both cortisol and androgen not only affects the body but may also impact a person’s mood. Excess cortisol results in stress, while excess androgen also results in obesity, acne, and hair loss. Ultimately, these symptoms may detrimentally affect a person’s self-image (Gnawali et al., 2021).
There are some limitations to this literature review. All the results were from a systematic review of previous studies. With that being said, this review does not include data from studies published in the current year. Moreover, all of the studies included were cross-sectional by design, which makes it difficult to understand how the relationship between PCOS and depression may change over time (Wang & Cheng, 2020). Furthermore, publication bias may have impacted the obtained results. The studies also did not account for the impact of additional external factors (e.g., natural disasters such as earthquakes, hurricanes, etc. ), which can lead to post-traumatic stress disorder, depression, and other mental disorders (Lenox). Finally, the studies included in this review consisted of small sample sizes, which may not be representative of the overall population.
Further research could explore whether these findings generalize to the entire population of women with PCOS. Cross-regional studies, research conducted across different geographical regions and/or healthcare systems, could be utilized to ensure that the findings are not centralized in one area. Additionally, the exact neurotransmitters and hormones that affect these women can also be examined.
Conclusion
This systematic review explores the relationship between Polycystic Ovary Syndrome and depression. Although the direct cause of depression and PCOS is unclear, common symptoms of PCOS, such as irregular menstruation, infertility, insulin resistance, etc., have been associated with heightened instances of depression (Xing et al., 2022). Additionally, excessive amounts of hormones such as cortisol and androgen can result in stress and decreased mood. Neurotransmitters, such as GABA, acetylcholine, and serotonin, play a key role in determining mood, and their levels are diminished (Xing et al., 2022). Overall, these findings contribute to the growing evidence that PCOS can affect mental health, particularly depression.
References
Dybciak, P., Raczkiewicz, D., Humeniuk, E., Powrózek, T., Gujski, M., Małecka-Massalska, T., Wdowiak, A., & Bojar, I. (2023). Depression in Polycystic Ovary Syndrome: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 12(20), 6446–6446. https://doi.org/10.3390/jcm12206446
Gnawali, A., Patel, V., Cuello-Ramírez, A., Al kaabi, A. S., Noor, A., Rashid, M. Y., Henin, S., & Mostafa, J. A. (2021). Why are Women With Polycystic Ovary Syndrome at Increased Risk of Depression? Exploring the Etiological Maze. Cureus, 13(2). https://doi.org/10.7759/cureus.13489
Hansson, M., Chotai, J., Nordstöm, A., & Bodlund, O. (2009). Comparison of two self-rating scales to detect depression: HADS and PHQ-9. British Journal of General Practice, 59(566), e283–e288. https://doi.org/10.3399/bjgp09x454070
Lichtenberg, P. (2010). Handbook of Assessment in Clinical Gerontology. Elsevier. https://doi.org/10.1016/c2009-0-01911-4
Maass, S. W. M. C., Roorda, C., Berendsen, A. J., Verhaak, P. F. M., & de Bock, G. H. (2015). The prevalence of long-term symptoms of depression and anxiety after breast cancer treatment: A systematic review. Maturitas, 82(1), 100–108. https://doi.org/10.1016/j.maturitas.2015.04.010
McCook, J. G., Bailey, B. A., Williams, S. L., Anand, S., & Reame, N. E. (2014). Differential Contributions of Polycystic Ovary Syndrome (PCOS) Manifestations to Psychological Symptoms. The Journal of Behavioral Health Services & Research, 42(3), 383–394. https://doi.org/10.1007/s11414-013-9382-7
Melo, A., Ferriani, R., & Navarro, P. (2015). Treatment of infertility in women with polycystic ovary syndrome: approach to clinical practice. Clinics, 70(11), 765–769. https://doi.org/10.6061/clinics/2015(11)09
Owens-Gary, M. D., Zhang, X., Jawanda, S., Bullard, K. M., Allweiss, P., & Smith, B. D. (2018). The Importance of Addressing Depression and Diabetes Distress in Adults with Type 2 Diabetes. Journal of General Internal Medicine, 34(2), 320–324. https://doi.org/10.1007/s11606-018-4705-2
Palomba, S., Santagni, S., Falbo, A., & La Sala, G. B. (2015). Complications and challenges associated with polycystic ovary syndrome: Current perspectives. International Journal of Women’s Health, 7, 745. https://doi.org/10.2147/ijwh.s70314
Pearson, S., Schmidt, M., Patton, G., Dwyer, T., Blizzard, L., Otahal, P., & Venn, A. (2010). Depression and Insulin Resistance: Cross-sectional associations in young adults. Diabetes Care, 33(5), 1128–1133. https://doi.org/10.2337/dc09-1940
Reuben, A., Schaefer, J. D., Moffitt, T. E., Broadbent, J., Harrington, H., Houts, R. M., Ramrakha, S., Poulton, R., & Caspi, A. (2019). Association of Childhood Lead Exposure With Adult Personality Traits and Lifelong Mental Health. JAMA Psychiatry, 76(4), 418. https://doi.org/10.1001/jamapsychiatry.2018.4192
Sam, S. (2007). Obesity and Polycystic Ovary Syndrome. Obesity Management, 3(2), 69–73. https://doi.org/10.1089/obe.2007.0019
Tremblay-Davis, A. C., Holley, S. L., & Downes, L. A. (2021). Diagnosis and Treatment of Polycystic Ovary Syndrome in Primary Care. The Journal for Nurse Practitioners, 17(10), 1226–1229. https://doi.org/10.1016/j.nurpra.2021.08.008
Triplitt, C. L. (2012). Examining the mechanisms of glucose regulation. The American Journal of Managed Care, 18(1 Suppl), S4-10. https://pubmed.ncbi.nlm.nih.gov/22559855/
Wang, X., & Cheng, Z. (2020). Cross-sectional studies: Strengths, weaknesses, and recommendations. Chest, 158(1), 65–71. NCBI. https://doi.org/10.1016/j.chest.2020.03.012
Woody, C. A., Ferrari, A. J., Siskind, D. J., Whiteford, H. A., & Harris, M. G. (2017). A systematic review and meta-regression of the prevalence and incidence of perinatal depression. Journal of Affective Disorders, 219(219), 86–92. https://doi.org/10.1016/j.jad.2017.05.003
Xing, L., Xu, J., Wei, Y., Chen, Y., Zhuang, H., Tang, W., Yu, S., Zhang, J., Yin, G., Wang, R., Zhao, R., & Qin, D. (2022). Depression in polycystic ovary syndrome: Focusing on pathogenesis and treatment. Frontiers in Psychiatry, 13. https://doi.org/10.3389/fpsyt.2022.1001484
